The Polio Vaccine
—Chrissie
Listen here: https://www.spreaker.com/user/bqn1/hwts208
In the first half of the twentieth century, the mere mention of Polio was enough to stop parents in their tracks. It was virulent, potentially debilitating, and sometimes deadly. Outbreaks closed schools, public parks, and anywhere else children might gather. It could also be difficult to identify a case, as it often presents with mild symptoms similar to those of a cold or flu, and most infections are asymptomatic. The disease spreads via bodily fluids and feces, infects via the mouth and develops in the gut; in most cases, it ends there. If, however, the disease attacks the central nervous system, it can cause muscle weakness and paralysis. This most often affects the legs, but if it spreads into the diaphragm and muscles of the chest, it can cause death by suffocation, when the muscles around the lungs stop functioning.
The disease is believed to have existed throughout human history; it is attested in texts and artwork going as far back as Ancient Egypt. It was first clinically described in 1789 and was often termed “infantile paralysis” because it primarily affects infants and small children. Epidemic outbreaks, however, are not seen until the late nineteenth century because it was endemic in pre-modern times with poor sanitation, meaning people developed immunity through exposure. Once clean water and better sanitation were the standard, there was no longer early exposure creating immunity.
Beginning with an 1894 outbreak in the United States, epidemics of polio were a regular occurrence across the industrialized world for the next seventy years. The virus mutated during these decades as well, more often infecting children between the ages of 5 and 10, rather than infants. Infections at this older age came with higher potential for disability and paralysis. Research on a vaccine began in the 1930s; in the US it centered on two researchers, Maurice Brodie of the New York City Health Department and John Kolmer at the Research Institute of Cutaneous Medicine in Philadelphia. Kolmer concentrated on a live virus vaccine and his work seemed successful, though his research and testing methods were questionable. He developed it in a haphazard way, trying various methods of isolating and attenuating (reducing the virulence of) the virus. In 1935, once he had a formula which he believed effective, he tested it on himself and his children. With good results, he expanded the trials, but conducted them with no control group and did not monitor the subjects beyond their vaccination and polio exposure.
Maurice Brodie worked on an inactive virus vaccine, beginning in 1933. They were aided by a grant from the President’s Birthday Ball Commission, a fundraising project to help those, like Franklin Roosevelt, who suffered from polio and its effects. This organization became the March of Dimes a few years later. Once Brodie was satisfied with his results, he experimented on himself and his family, then moved to trials with local children. The US Public Health Service also tested it with an outbreak in Kern County, California. The Brodie formula was promising and seemed to be effective with few side effects.
Both Kolmer and Brodie presented their work at a meeting of the American Public Health Association in October of 1935. At the meeting, their bacteriologist colleagues presented them with a long list of the faults in the methods both men had used, which they believed brought not only the results into question but also left them concerned with the safety of the vaccinations. In fact, Kolmer’s vaccine had been withdrawn from use just before the meeting due to incidences of paralytic polio appearing in his test subjects. Brodie’s was much safer and had a better record, but three incidences of paralysis in children who received the vaccine caused his to be pulled in December 1935. Its efficacy was proven by its use as a basis for Jonas Salk’s successful vaccine two decades later.
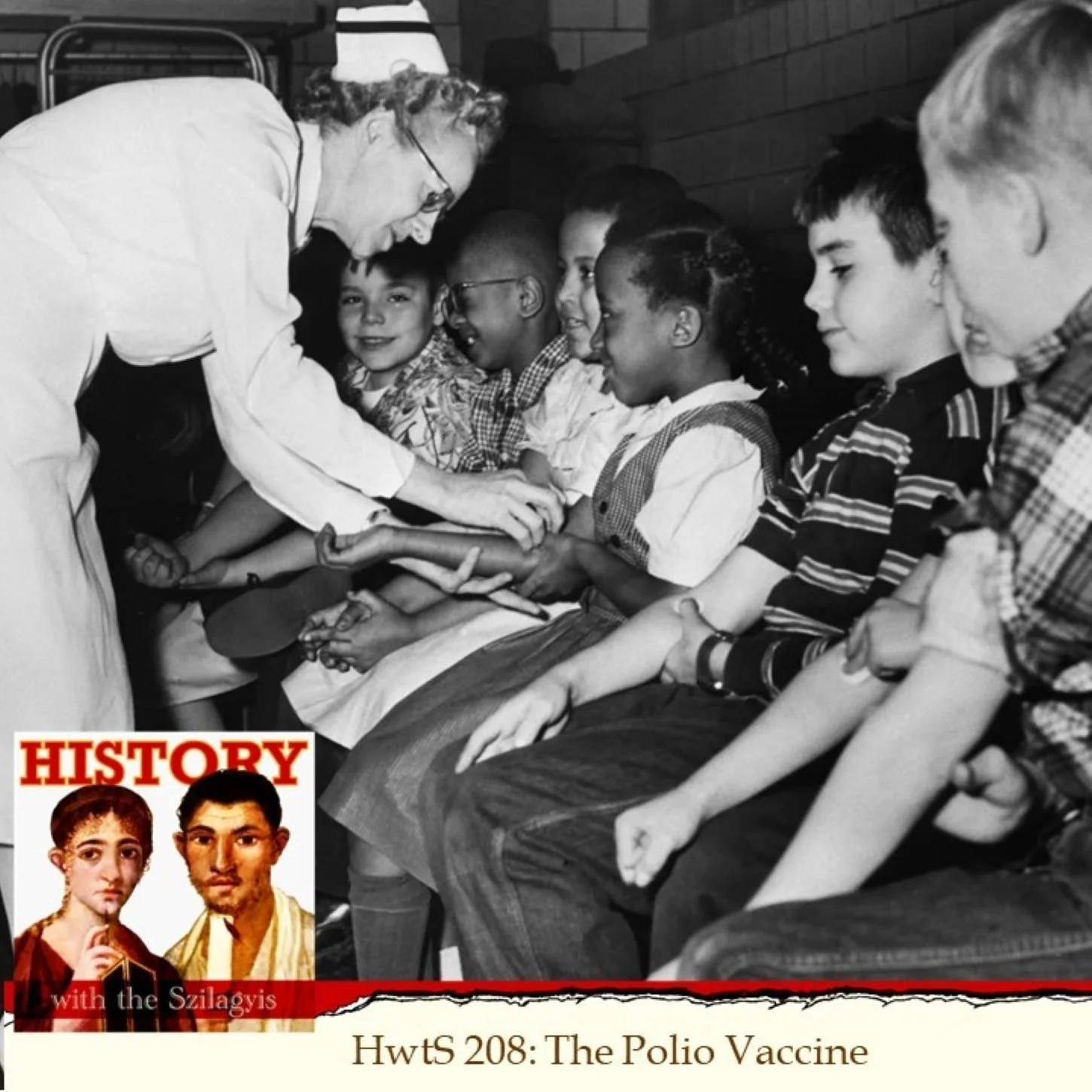
In 1949, a group of researchers at Boston Children’s Hospital, John Enders, Frederck Robbins, and Thomas Weller, were able to cultivate the virus in human tissue samples, allowing for easier and more accurate testing of vaccines. Jonas Salk and his team used this to develop their formula at the University of Pittsburgh in the early 1950s. He announced a small successful trial in March 1953, which was followed by mass production for a larger trial conducted over the next two years. After these proved massively successful, the Salk vaccine was approved for general use and was administered to children across the US beginning in late 1955. Because of Salk’s work, the polio numbers in the United States went from 35,000 in 1953 to 5600 in 1957. Fewer than two hundred cases were reported in 1961.
Salk’s vaccine was superseded in a few years by an oral vaccine developed by Albert Sabin and Hilary Kapowski. There were two reasons for this: the first is that the new vaccine was much easier to administer; most commonly the solution was dripped onto sugar cubes which children happily ate. The second reason was an improperly prepared batch of the Salk vaccine from Cutter Laboratories which caused many infections and eleven deaths.
Over the next few decades, incidents of polio infection worldwide reduced dramatically due to expanded vaccination. The Americas were declared polio-free in 1994, China and Australia in 2000, most of Europe by 2002, and India in 2012. That doesn’t mean, though, that people in these places no longer need to be vaccinated; unlike a disease like smallpox which can be fully eradicated by ending all infections, polio occurs in nature and so can appear in unvaccinated populations at any time. There are also many places in the world in which people are not vaccinated where the disease still runs rampant. The best way to assure that you and your loved ones never have to be concerned about polio is to vaccinate.